At Lightyear Health, we’re helping the millions of people living with functional decline from aging and complex medical illness in post-acute settings like skilled nursing facilities. Our Lightyear Health Clinics bring modern physiatry (physical medicine and rehabilitation) care to patients and families everywhere.
Trusted by medical providers around the US

Our Lightyear Health Clinics support the unique healthcare needs of seniors and those facing complex medical illness with dedicated and regular in-person services which put the patient and their needs at the center of our service.
Our physical medicine & rehabilitation (PM&R) physician specialists bring the latest advancements in medicine and technology to improve the functional and physical health of seniors.
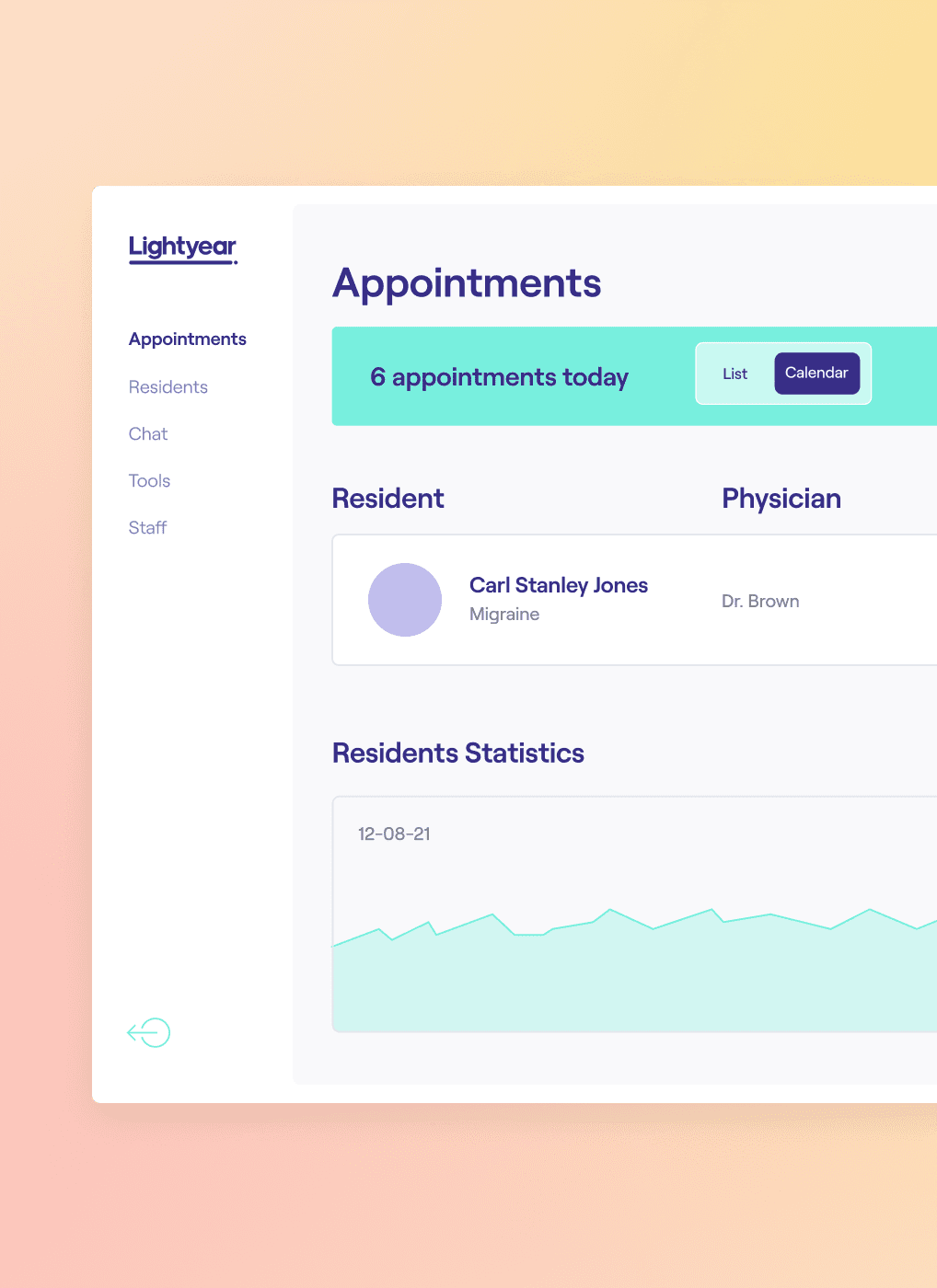
The Lightyear Health Clinics use modern technologies and solutions to ensure that all of our patients, families, and partner facilities experience precise, seamless care.
We help care providers, community staff, patients, and family members work together proactively to slow down functional decline and extend quality of life.

“Donec sed odio dui. Duis mollis, est non commodo luctus, nisi erat porttitor ligula, eget lacinia odio sem nec elit.”
Peter Newman, CEO


© 2022 Lightyear Health Inc.
We’re focused on making our website accessible and functional for all our users, including those who may have disabilities. In doing so, we look to the Web Content Accessibility Guidelines (WCAG) 2.0, Levels A and AA. We primarily use automated tools to assist in assessing and in improving the accessibility of our website. We view accessibility as an ongoing effort, and if you encounter an accessibility issue please contact us at at 818-575-6351 to work with you to resolve the issue.